Hemorrhoids: Types, Features, and Management
- Mayta

- May 27, 2024
- 3 min read
Updated: Oct 2, 2025
Hemorrhoids: Types
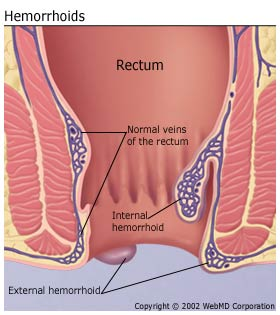
Internal hemorrhoids
Originate above the dentate line (from the superior rectal venous plexus).
Covered by columnar epithelium → not painful (no somatic innervation).
Symptoms: painless bright red bleeding, prolapse, mucus discharge, and pruritus.
External hemorrhoids
Originate below the dentate line (from the inferior rectal venous plexus).
Covered by anoderm/skin → richly innervated → painful.
Symptoms: acute pain, swelling, and may thra ombose (bluish perianal lump).
Differentiating Internal vs. External
Feature | Internal Hemorrhoid | External Hemorrhoid |
Location | Above the dentate line | Below the dentate line |
Epithelium | Columnar (insensate) | Squamous/skin (sensitive) |
Pain | ❌ Painless | ✅ Painful, esp. thrombosis |
Main Symptom | Bleeding, prolapse | Perianal pain, swelling |
Exam | Seen on anoscopy | Visible on inspection |
Grading of Internal Hemorrhoids (by degree of prolapse)
(Most widely used = Goligher’s classification)
Grade I:
Hemorrhoids protrude into lumen but do not prolapse outside the anal canal.
Present with painless rectal bleeding only.
Grade II:
Hemorrhoids prolapse outside anal canal during defecation but reduce spontaneously.
Grade III:
Hemorrhoids prolapse during defecation or exertion and require manual reduction.
Grade IV:
Hemorrhoids irreducibly prolapsed, permanently outside the anal canal.
May become thrombosed or strangulated.
📌 Mnemonic:
I = In (never prolapse).
II = Out, In (comes out but goes back in by itself).
III = Out, Need Hand In (manual reduction needed).
IV = Always Out (irreducible).
Thrombosed External Hemorrhoid
Definition: Acute clot (thrombus) formation within an external hemorrhoidal vein (below dentate line).
Pathophysiology: Sudden venous rupture → blood clot trapped under skin → intense perianal pain.
Clinical features:
Severe acute pain (esp. during sitting, coughing, defecation).
Tender bluish perianal nodule (subcutaneous).
Swelling, difficulty sitting.
Pain peaks in first 48–72 hrs, then gradually improves.
Management:
If <72 hrs: Excision under local anesthesia (thrombectomy) → immediate pain relief.
If >72 hrs: Conservative (analgesics, sitz baths, stool softeners, Daflon).
Acute vs. Chronic Hemorrhoids
Acute Hemorrhoids
Sudden onset, often due to thrombosis.
Severe pain (esp. external).
Perianal swelling, tender bluish nodule.
Acute bleeding is possible.
Usually self-limited but very symptomatic.
Chronic Hemorrhoids
Long-standing, recurrent symptoms.
Painless rectal bleeding during defecation.
Prolapse (grades II–IV).
Pruritus ani, mucus discharge, soiling.
Pain only if thrombosed or strangulated.
Cut-off Between Acute vs. Chronic Hemorrhoids
Acute Hemorrhoids
Definition: New, sudden event, usually due to thrombosis or strangulation of a hemorrhoidal vein.
Time course: Symptoms develop within hours to days.
Main hallmark: Severe pain + perianal swelling (external or prolapsed thrombosed internal).
Course: Self-limited, resolves in days to ~2 weeks, even without surgery (though excision may speed recovery).
👉 Cut-off: Acute = Thrombosed or strangulated hemorrhoid with symptoms < 2 weeks.
Chronic Hemorrhoids
Definition: Long-standing vascular cushion enlargement with recurrent symptoms.
Time course: Symptoms persist or recur for weeks to months.
Main hallmark:
Painless rectal bleeding during/after defecation.
Prolapse (graded I–IV).
Mucus discharge, pruritus, soiling.
Pain only if thrombosed (then → acute flare on chronic).
👉 Cut-off: Chronic = Recurrent or persistent symptoms > 2 weeks with structural changes (bleeding, prolapse, pruritus, mucus).
✅ Hemorrhoids Management
1. Conservative / Medical Management
Indicated for:
Grade I–II internal hemorrhoids.
External hemorrhoids (non-thrombosed).
Chronic hemorrhoids without severe prolapse.
Measures:
Lifestyle: High-fiber diet (20–35 g/day), hydration, avoid straining, regular exercise.
Sitz baths: 10–15 min × 2–3/day.
Stool softeners/laxatives: Docusate, PEG.
Medications:
Daflon (MPFF) – venotonic, reduces bleeding/inflammation.
Topical hydrocortisone, lidocaine, and witch hazel.
NSAIDs / acetaminophen for pain.
2. Office-Based / Minimally Invasive Procedures
Indicated for:
Grade II–III internal hemorrhoids refractory to conservative therapy.
Options:
Rubber band ligation (most effective for Grade II–III).
Sclerotherapy (phenol injection).
Infrared coagulation / bipolar diathermy.
3. Surgical Management (Hemorrhoidectomy / Stapled Hemorrhoidopexy)
Indicated for:
Grade IV internal hemorrhoids (irreducible prolapse).
Large Grade III hemorrhoids not responding to rubber band ligation.
Thrombosed external hemorrhoid (within 72 hrs of onset → excision under local anesthesia).
Recurrent bleeding with anemia.
Mixed hemorrhoids (internal + external).
Surgical Options:
Excisional hemorrhoidectomy (Milligan-Morgan or Ferguson) – gold standard for advanced hemorrhoids.
Stapled hemorrhoidopexy – for circumferential prolapse.
Thrombectomy – for acute painful thrombosed external hemorrhoids (<72 hrs).
High-Yield
Grade I–II → Medical/office procedures.
Grade III → Start with rubber band ligation; surgery if refractory.
Grade IV → Surgery definitive.
Thrombosed external hemorrhoid → excision if <72 hrs (best pain relief).
In summary:
Medical + lifestyle → Grades I–II.
Office procedures → Grade II–III.
Surgery → Grade IV, large/refractory Grade III, thrombosed external hemorrhoids, recurrent severe bleeding.





Comments